Conference Information
Welcome Message
Arthroplasty 2022 welcomes all the eminent speakers and guests from all over the country for the 15th International Conference on “Orthopaedics, Arthroplasty and Arthroscopy” to be held on September 19-20, 2022 through a webinar.
It is our great pleasure to warmly invite Orthopaedics, Arthroplasty and Arthroscopy Experts and Researchers, Academicians, Scientists, Industry Professionals and students and other associated individuals to this webinar.
Attending Arthroplasty 2022 webinar, people will get a chance to network with leading scientists and business specialists, as well as investors which will help to exchange ideas and expert opinions and present their research work to a global network
Arthroplasty 2022 will cover a wide range of topics related to Orthopaedics, Arthroplasty arthroscopy including causes, types, and rehabilitation treatments. Arthroplasty 2022 webinar will feature 16 sessions with keynote speakers, presenters, and research forums.
We'd like to extend an invitation to our fascinating webinar and extend a warm welcome to you.
About Conference
Arthroplasty 2022 takes immense pleasure in inviting all the participants from across the globe to attend “15th International Conference on Orthopaedics, Arthroplasty and Arthroscopy” during September 19-20, 2022, through webinar. The conference comprises eminent personalities with their keynote presentations, verbal speeches, productive poster presentations and exhibitions along with a discussion forum providing the insights on the advances of the Arthroplasty.
Arthroplasty 2022 is an International gathering organized by Pulsus, that unites all the innovators to glaze the entire field of Arthroplasty and to experience the advancements in the research and development in the field of Orthopedics, Orthopedics Surgery, Podiatry, Foot-care, Hand-care, Arthritis, Osteoporosis, Rheumatology, Sport-Medicine, Paediatric Orthopedics, Orthopedics & Trauma, Bone health and many more.
The event comprises the various aspects of arthroplasty with discussion on causes and types of Arthroplasty and Arthroscopy with their Rehabilitation methods. The new emerging prosthesis with applied technologies of Biomaterials, Nanotechnology, Ayurveda and Tissue engineering in Orthopedics are comprised in the conference.
Arthroplasty 2022 provides scope and experience for all eminent participants to explore the advancements in the field of Arthroplasty and Arthroscopy and to expose their research work across the global network and expose an international gathering on life science and Surgery.
We hope to see you and look forward to sharing new information and exciting discoveries with you.
Regards,
Arthroplasty 2022 | Organizing Committee Member
Scientific Sessions
Session 01: Orthopaedics
It is a branch of surgery which focus on injuries and the disease of the musculoskeletal system. Musculoskeletal system is a complex system that includes bones, joints, ligaments, tendon muscles and nerves. After proper diagnosis and consultation orthopaedic surgeons treat problems of the musculoskeletal system like musculoskeletal trauma, spine disease, sport injuries, infection, tumour and congenital disorder by both surgical and non surgical method.
- Upper extremity and hand
- Paediatric orthopaedics
- Orthopaedic oncology
- Dermatology in orthopaedics
- Shoulder and elbow
Session 02: Clinical diagnosis of Orthopaedic
To diagnose and screen for orthopaedic problems, a range of tests can be employed. Some diagnostic tests can assist to identify the exact location and severity of the problem. Bone densitometry, skeletal scintigraphy, discography, myelography, and electromyography are all common orthopaedic examinations. In some circumstances, additional tests, such as muscle biopsy and bone marrow biopsy may be required.
Session 03: Orthopaedics Surgery
Non-surgical method- musculoskeletal disorder can be treated without surgery. Orthopaedic surgeons might recommend medicine, exercise, rehabilitation, or other therapies as part of a therapy plan. If non surgical therapy not effective for the disorder surgeon may recommend surgery.
Surgical method- A surgeon who specializes in orthopedics can undertake a variety of procedures. Some of the most popular techniques are Arthroscopy, Joint replacement, Fusion, osteotomy and Internal fixation.
- ACL Reconstruction Surgery
- Ankle Repair and Spinal Surgeries
- Limb reconstruction surgery
- Orthopaedics Medical Devices
- Orthopaedics: Diagnostic Techniques
Session 04: Osteoporosis
A condition in which the bones become brittle and fragile. Osteoporosis causes porous or weak bones, which raise the risk of fractures, especially in the hip, spine, and wrist bones. Osteoporosis affects around 2 million men over the age of 65 but it is more common in older women. Osteoporosis is a condition that goes unnoticed. It's possible that you won't realise you have it until you break a bone.
The best way to monitor your bone health is to have a bone mineral density test. To keep your bones strong eat a calcium and vitamin-D-rich diet, exercise regularly, and avoid smoking. Men and women between the ages of 18 and 50 should consume 1,000 mg of calcium every day. This daily dose rises to 1,200 mg once women reach 50 and males reach 70.
- Risk Factors of Osteoporosis
- Research Progress Related to Osteoporosis
- Osteoporosis Medication
- Conventional Treatment for Osteoporosis
- Osteoporosis symptoms
- Senile osteoporosis
Session 05: Arthroplasty
Arthroplasty is a type of orthopaedic surgery in which the articular surface of a musculoskeletal joint is replaced, modified, or realigned using osteotomy or another method .For example, an osteoarthritic hip joint can be completely replaced with a prosthetic hip (total hip arthroplasty).
According to the American Academy of Orthopaedic Surgeons (AAOS) more over 7 million people in the United States have an arthroplasty . The most successful and prevalent type of arthroplasty for the past 45 years has been the surgical replacement of arthritic or joint surface with a prothesis. Hip and knee arthroplasties are the two most common surgeries in the United States, with up to one million procedures performed each year.
- Silicone replacement arthroplasty
- Mold arthroplasty
- Interpositional arthroplasty
- Joint treatment and Replacement
- Orthopedics trauma
Session 06: Osteoarthritis
Also known as degenerative joint Disease , it is the most common type arthritis. Osteoarthritis is a degenerative condition of the articular cartilage that is characterized with hypertrophic bone alterations. Although the damage to joints cannot be repaired, the symptoms of osteoarthritis can typically be treated. Staying active, eating a healthy diet, and receiving specific treatments may help reduce disease development and improve pain and joint function.
Around 80% of elderly people aged 55 and up, have osteoarthritis as evidenced by X-ray. Symptomatic osteoarthritis impacts 240 million adults globally, including more than 30 million adults in the United States. In comparison to men, Knee osteoarthritis was shown to be more common in postmenopausal women than in males.
- Medications
- Lifestyle and home remedies Complications of osteoarthritis
- Osteonecrosis
- Risk factors of Osteoarthritis
Session 07: Rheumatoid Arthritis (RA)
Rheumatoid arthritis (RA) is an autoimmune and inflammatory disease in which your immune system mistakenly affects healthy cells in your body, resulting in inflammation (painful swelling) in the affected areas .Hands, knees, and ankles are the most prevalent sites for the disorder, and it usually affects the same joint on both sides of the body, such as both hands or both knees.
RA affects more women than males for unspecified reasons, and it usually manifests in middle life. Researchers are confused as why people get Rheumatoid Arthritis. They believe these people have genes that are activated by a trigger in the environment, such as a virus or bacteria, physical or emotional stress, or another element.
- Research and new developments
- disease-modifying anti-rheumatic drugs (DMARDs)
- Biologic treatments
- Rheumatic Diseases
- Clinical Rheumatology
Session 08: Knee Arthroplasty
Knee arthroplasty commonly known as complete knee replacement, is a surgical surgery that resurfaces a knee that has been affected by arthritis The ends of the bones that shape the knee joint are capped with metal and plastic components. To determine if a knee replacement is right for you, an orthopaedic surgeon assesses your knee's range of motion, stability, and strength. X-rays assist in the detection of damage.
Knee replacement surgery may be an option if medicinal therapy is inadequate. In the United States, knee replacement surgery is one of the most common bone surgery. Every year, more than 600,000 knee replacement procedures are performed in the United States, with many of them now being performed robotically.
- Surgical Techniques for Knee Replacement
- Inflammatory arthritis
- Trauma
- TKA and TKR
Session 09: Shoulder Arthroplasty
Shoulder arthroplasty (TSA) is a procedure that restores the glenohumeral joint to its original state, which includes both the upper edge of the humerus and the glenoid. While shoulder joint replacement is not as common as knee or hip replacement, it is equally effective in relieving joint discomfort. According to the Agency for Healthcare Research and Quality, about 53,000 people in the United States receive shoulder replacement surgery each year. In comparison, almost 900,000 Americans get knee and hip replacement surgery each year. It primarily affects those over the age of 50, but younger people can also be affected.
- Hemiarthroplasty
- Total shoulder arthroplasty(TSA)
- A reverse total shoulder arthroplasty (rTSA)
- Shoulder Arthroplasty in fractures
Session 10: Hip Arthroplasty
Common actions like walking or stepping in and out of a chair may be uncomfortable and difficult if your hip has been injured by arthritis, a fracture, or other disorders. It's possible that your hip is stiff, making it difficult to put on your shoes and socks. It's possible that you'll feel anxious while relaxing. If drugs, lifestyle changes, and the use of walking aids aren't enough to relieve your symptoms, hip replacement surgery may be an option.
As per Agency for Healthcare Research and Quality In the United State, more than 450,000 total hip replacement are performed each year The decision to have surgery is made based on the patient's difficulty and impairment, not their age. The majority of patients who have a total hip replacement are between the ages of 50 and 80, although orthopaedic surgeons assess each patient individually.
- Hip preservation Surgery
- Implant Components
- Possible Complications of Surgery
- Childhood hip disease
- Hemiarthroplasty
Session 11: Spine Surgery
Traditionally, spine surgery has been done as an "open procedure." This entails making a wide incision in the area to be operated on to allow the surgeon access. In recent years, technological advancements have made it possible to treat more back and neck disorders with a minimally invasive surgical method. Minimally invasive spine surgery (MISS) minimises significant damage to the muscles surrounding the spine because it does not require a major incision. This usually leads to less discomfort and a quicker recovery.
- Minimally invasive spine surgery (MISS)
- Spinal instrumentation
- Spinal Osteoarthritis
- Spondylolysis
- Spinal stenosis
Session 12: Anterior Longitudinal Ligament
The anterior longitudinal ligament is a ligament that runs down the spine's anterior surface. Over the vertebral bodies, the ligament is thicker and narrower, whereas over the intervertebral discs, it is thinner and wider. In comparison to the posterior longitudinal ligament, this effect is significantly lesser pronounced. Between two adjacent vertebrae, the anterior longitudinal ligament can be "released," or partially cut to treat abnormalities in vertebral column curvature, such as kyphosis. The ACR method employing anterior longitudinal ligament release should not be utilised in patients with osteoporosis or osteopenia because it increases the risk of spacer sinking through the end plates.
The ossification of the anterior longitudinal ligament (OALL) is generally thought to be the cause of Diffuse idiopathic skeletal hyperostosis (DISH). Dysphagia can be caused by Diffuse idiopathic skeletal hyperostosis (DISH) and cervical ossification of the anterior longitudinal ligament (C-OALL) .Conservative treatment is normally chosen, but if the condition does not improve, surgery may be necessary. In the current research study, Four human cadaveric spines were frozen and sectioned using a cryomacrotome after being identified with DISH using CT imaging.
- Diffuse idiopathic skeletal hyperostosis (DISH)
- Lumbar vertebrae
- Spondylosis
- Cervical vertebrae
- Cervical Lordosis
Session 13: Arthroscopy
It is a keyhole procedure for the diagnose and treatment of joints. Knees, ankles, shoulders, elbows, wrists, and hips are the most common places where it's applied. It is performed to determine the level of joint damage caused by injuries like sports injuries and others. The doctor makes a series of small incisions (cuts) across the knee before inserting the arthroscope (a small tube-like tool) into the joint. It has some advantage over open surgery” Because the arthroscopy equipment is so small, only little skin cuts are required. Knee Arthroscopy
- Diagnostic and Treatment
- ECL OR PCL
- Acromegaly
- Infections in Arthroscopy
Session 14: Consequence of Arthroscopy
The overall risk of problems linked with knee arthroscopy has been calculated to be around 5%. The chances of a major complication from knee arthroscopy are fewer than 1%. Although the most common surgical risks are not life-threatening, they can be unpleasant. Infection, nerve damage, blood clots, chronic swelling and stiffness, heart attack, and stroke are all risks and complications of arthroscopic knee surgery.
- Localized soft tissue infection
- Leg vascularity seems to be poor.
- Clots in the blood
- Infection
Session 15: Exercise and Sports Medicine
Orthopaedic medicine is a type of medicine that focuses on the function of the musculoskeletal system. Orthopaedic sports medicine is dealing with the prevention and treatment of musculoskeletal injuries caused by athletics activity. Specialists in this profession are aware with diseases affecting the bones, joints, tendons, ligaments, and muscles, and they can treat these problems with a range of approaches, including drugs, physical therapy, corrective braces, and surgery.
- Sports medicine organizations
- Nutritionists
- Exercise induced bronchospasm
- Rehabilitation Methods
Session 16: Case report of orthopaedics
The annual number of total knee arthroplasties (TKAs) is gradually increasing. There are no strict rules for long-term follow-up after these arthroplasties. Therefore recommendations for clinical follow-up guidelines are disputed. Although a few case series have been published that indicate a small percentage of patients who require revision TKA for aseptic loosening or discomfort more than 15 years after their index surgery, no published research have yet documented these patients or the pathology present at the time of surgery in detail.
Session 17: Impact of Covid 19 (orthopaedic)
The COVID-19 epidemic had a significant impact on orthopaedic doctors, as well as orthopaedic residents, who are the backbone of any department or institution. This COVID 19 pandemic situation is also affecting orthopaedic residents, since they are not getting enough surgical exposure and hands-on training because regular procedures are being cancelled or postponed at this time. Most orthopaedic subspecialty surgeries, such as joint replacement, arthroscopy, and sports injury surgery, as well as elective spine and deformity correction surgeries are postponed or cancelled since they are not emergencie
Market Analysis
MARKET OVERVIEW OF ORTHOPAEDICS DEVICES
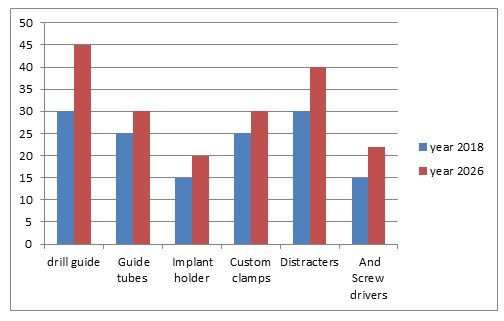
In 2018, the global orthopaedic devices market reached $37.2 billion, and by 2026, it is predicted to be around $47.7 billion, registering a compound annual growth rate (CAGR) of 3.1% from 2019-2026. Orthopaedics device manufactured to support a damaged bone by replacing the damaged part of the bone and re-establish the natural function of the skeleton. According to the World Health Organization (WHO) 2017, Musculoskeletal disorders are becoming more common as people become older, and In the East Mediterranean and African regions, the musculoskeletal condition was excessive. It is vary Due to differences in environmental, racial, and geographic factors.
COVID-19 has caused massive disturbance in healthcare workflows around the world. Various industries, including several sub-domains of health care, have been forced to close their doors temporarily because to the disease. According to the Commonwealth Fund, it is expected to result in a roughly 60% reduction in overall outpatient visits by May 2020, due to Covid 19.
According to the paper published in Europe PMC pandemic has impacted outpatient clinics, emergency and elective surgery, rehabilitation, resident training, personnel management, the usage of personal protective equipment, telemedicine etc.
According to the Arthritis Foundation, 30.8 million adults in the United States were diagnosed with arthritis in 2019, and 14 million people were diagnosed with symptomatic knee osteoarthritis. By 2050, the number of adults in the United States with osteoarthritis diagnosed by a doctor is expected to go up by 49 percent to 78.4 million. The number of persons who have activity limits as a result of arthritis will rise by 52% to 34.6 million.
Review by Product segment:
Various products comes under the orthopaedic devices category like
• Drill guide
• Guide tubes
• Implant holder
• Custom clamps
• Distracters
• And Screw drivers.
In 2018, the drill guide segment held the greatest share, and it is expected to maintain this trend and increase rapidly during the forecast period.
By Product
Review by Application segment:
Based on application orthopaedic device market includes
• Hip orthopaedic device,
• Knee orthopaedic device ,
• Spine orthopaedic device,
• Craniomaxillofacial orthopaedic device,
• Dental orthopaedic device,
• Sport injuries and extremetie And trauma orthopaedic device.
By Region:
Based on region the orthopaedics device market is analysed around North America, Europe, Asia –pacific and LAMEA. According to the data of 2018, North America led the worldwide orthopaedic device market and this trend is expected to continue during the forecast period. However, because to a growth in metabolic disorders, a large population base, high disposable income, and improved patient awareness about the adoption of orthopaedic devices goods, Asia-Pacific is predicted to have a high CAGR during the projection period.
1. North America
- U.S
- Canada
- Mexico
2. Europe
- German
- France
- Spain
- Italy
- UK
- Rest of Europe
3. Asia –pacific
- Japan
- India
- Australia
- China
- Rest of Asia-pacific
4. LAMEA
- Brazil
- Saudi Arabia
- South Africa
- Rest of LAMEA
Who To Attend?
- Orthopedics Surgeons
- Sports Medicine Doctors
- Trauma Surgeons & Specialists
- Orthopaedic Nurses
- Spine Surgeons
- Foot and Ankle Surgeons
- Shoulder and Upper Limb Surgeons
- Intensivists
- Emergency Medicine Doctors
- Orthopedics resident
- Physiotherapists
- Pain Therapists
- Medical Students
- Rheumatologists
- Manufacturing Medical Devices Companies
- Business Entrepreneurs and Industry professionals